


Serotonin
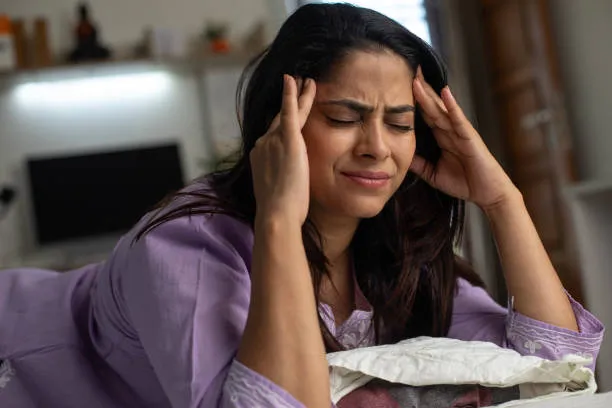
Migraines are intricate neurological conditions characterized by headaches, light and sound sensitivity, nausea, and cognitive issues. Studies indicate that serotonin (5-HT) significantly contributes to the onset of migraines.
How Serotonin Influences Migraines
Serotonin plays a crucial role in managing pain, blood vessel activity, and inflammation within the brain. Fluctuations in serotonin levels can instigate migraines through various pathways:
Serotonin Levels Decline Prior to a Migraine Attack
Serotonin Impacts Pain Sensitivity
Serotonin Imbalance Provokes Inflammation
Serotonin Governs Sleep and Mood

Dopamine
Migraines are intricate neurological occurrences, and the dysregulation of dopamine significantly influences their development and symptoms. Dopamine impacts blood vessel tone, pain perception, and sensory sensitivity—all crucial elements in migraines. During an episode, dopamine levels may vary erratically, leading to symptoms such as nausea, visual disturbances, mood fluctuations, and heightened sensitivity to light or sound. Some people might also suffer from dopamine hypersensitivity, where typical dopamine activity provokes migraine symptoms. Factors like stress, hormonal shifts, inadequate sleep, or specific foods can disturb dopamine equilibrium and trigger a migraine.
Noradrenaline
Noradrenaline functions as both a hormone and a neurotransmitter that plays a crucial role in the fight-or-flight response. It is synthesized in the brainstem, particularly in the locus coeruleus, as well as in the adrenal glands. This compound influences various bodily functions, including blood vessel constriction, heart rate, sleep-wake cycles, and the perception of pain.
How Noradrenaline Relates to Migraines
Pain Modulation
Noradrenaline plays a key role in modulating pain via descending pain-inhibitory pathways located in the brainstem.
When noradrenaline activity is low, the effectiveness of these inhibitory pathways may diminish, leading to increased pain sensitivity during migraine episodes.
Low initiative, even for activities you find enjoyable.
Struggles with maintaining focus or completing tasks.
A pervasive feeling of “why bother?”
Vascular Effects
Migraines, especially those accompanied by aura, are associated with alterations in cerebral blood flow.
Noradrenaline induces vasoconstriction, which is the narrowing of blood vessels. An imbalance in noradrenaline levels could result in abnormal vascular responses, potentially triggering or exacerbating migraines.
Stress and Cortisol Link
Stress is a well-known trigger for migraines, and noradrenaline serves as a primary chemical involved in the stress response.
Chronic stress can lead to elevated levels of noradrenaline, which may sensitize neurons, heighten inflammation, and contribute to central sensitization, a significant characteristic of chronic migraines.
Sleep and Wakefulness
Noradrenaline is vital for the regulation of REM sleep and maintaining alertness.
Disrupted sleep patterns or poor sleep quality are recognized triggers for migraines, likely due to an imbalance in noradrenaline levels.
Trigeminal Nerve Interaction
The trigeminal nerve plays a significant role in the experience of migraine pain.
Noradrenaline affects this system and can either reduce or enhance nociceptive (pain) signals, depending on which receptor subtypes are activated.
Migraines are not merely intense headaches; they are intricate neurological occurrences often influenced by hormonal fluctuations. If you suffer from chronic migraines, when these hormones become unbalanced, your brain's sensitivity to pain, light, sound, and stress increases—setting the stage for migraines.
Adrenaline
Adrenaline acts as your body's emergency response mechanism. It enables you to cope with stress, but an excess or deficiency can have adverse effects—particularly on your brain.
In Migraine:
Common Patterns:
GABA: Your Brain’s Off Switch
GABA serves as the calming neurotransmitter that aids your brain in slowing down, resting, and recuperating.
In Migraine:
Common Patterns:
Glutamate
Glutamate is the primary excitatory neurotransmitter in the brain—it energizes neuron activity and is crucial for pain perception, sensory processing, and vasodilation (the widening of blood vessels).
Glutamate's Role in Migraine
Inducing Cortical Spreading Depression (CSD)
Sensory Overload & Pain Amplification
Sensory Overload & Pain Amplification
This results in:
Glutamate and Chronic Migraine
Research indicates that individuals suffering from chronic or frequent migraines have consistently high levels of glutamate in their cerebrospinal fluid and blood.
This ongoing glutamate surplus results in: